T Cells play a critical role in cell-mediated immunity and arise from lymphoid progenitor cells that originally developed from hematopoietic stem cells in the bone marrow.
T Cells are identified by the expression of CD3 and develop into their various subtypes in the thymus (hence the name T Cell). Each subtype is defined by the specific receptors expressed on the cell surface, making these cells highly selective to non-self pathogens. Mature T Cells are released into the bloodstream where they can be induced to become one of several classes of T cells including:
T Cells become activated when a pathogenic antigen binds their cell-surface receptors. Each cell-surface receptor has affinity to a unique antigen, making T Cells highly specialized in antigen recognition.
Once the T Cell receptors bind an antigen, the T Cell will activate a series of internal signaling pathways that allow for the antigen recognition to be verified. Only then will the T cell proliferate, expanding the pool of available cells that are specific for the harmful antigen, such as to different bacteria and parasites.
CST has a wide array of expertly validated antibodies that can distinguish T cell populations accurately and reproducibly by WB, IF/IHC, IP and extracellular/intracellular flow cytometry.
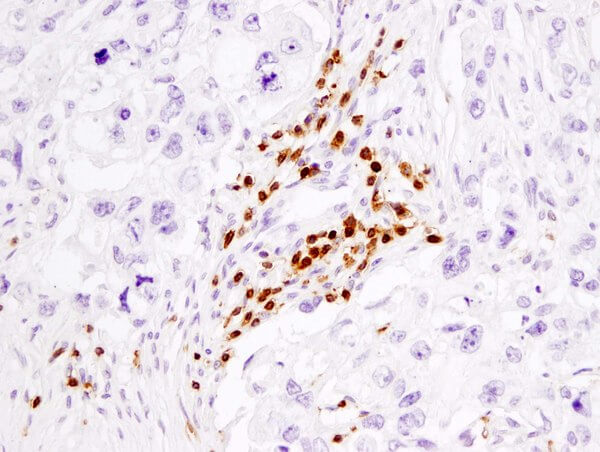
Using specific antibodies, individual subtypes of T Cells can be distinguished from a heterogeneous pool of immune cells. This type of immune cell subtyping is known as immunophenotyping.
Immunophenotyping of T Cells can be accomplished because T Cells have specific cell surface receptors, intracellular cytokine expression profiles, and/or differential phosphorylation of other intercellular proteins. This allow for selective labeling of these cells with specific markers. T Cells can first be immunophenotyped using IHC methods based on their CD3 expression, then they can be further sub-classified based on other well-characterized markers.